
PCOS

Dr David Richardson
Polycystic Ovary Syndrome (PCOS) Spectrum
Polycystic Ovary Syndrome affects between 5% and possibly up to 20% of all women sometime in their life.
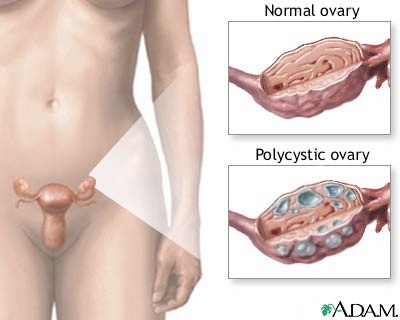
Not all women with PCOS have ovarian cysts, and not all women with multiple ovarian cysts have PCOS.
PCOS is a highly variable spectrum of symptoms, and is vastly under diagnosed by doctors. Many women with PCOS visit GPs, dermatologists, gynaecologists and even fertility clinics and have symptoms of their condition e.g. acne or infertility treated without ever being diagnosed with PCOS.
Understanding the diagnosis of PCOS and what it means empowers women who have this condition. It enables them to understand their condition and why they seem different to other women and girls. Diagnosing women with PCOS enables them to make the lifestyle decisions about diet and exercise and family planning which are absolutely essential to the successful management of PCOS.
If a woman with PCOS is not told that this is their diagnosis, she is denied the chance to self manage her condition. Withholding the diagnosis infringes this right, and possibly denies her maximising the chance of having children.
PCOS is essentially a different sex hormone balance to the normal female balance. Many women with PCOS flip from the normal balance to the PCOS balance according to lifestyle factors such as weight gain, diet & stress. Equally with lifestyle changes they can also flip back to the more common balance of female hormones.
PCOS MAY cause some of the following problems, in various combinations:
Effects of PCOS Spectrum
-
•Early start of menstruation (menarche), often younger than 12
-
•Rapid weight gain and change in body type from lean to heavier coinciding with pre-puberty
-
•Irregular periods which may persist longer than the normal first 1-2 years after puberty
-
•Acne which may persist into adulthood
-
•Increased body and facial hair (hirsutism)
-
•Loss of head hair, often starting with thinning in the temples. This is not pronounced in young women and girls.
-
•Multiple cysts in the ovaries.
-
•Central obesity (more fat round the tummy area, butts and thighs)
-
•Sugar, carbohydrate and chocolate cravings
-
•Increased levels of circulating insulin related to:
-
◦Increased resistance to Insulin i.e. reduced sensitivity to Insulin
-
◦Increased risk of diabetes or prediabetes or gestational diabetes
-
•Increased levels of male hormones (androgens), specifically Testosterone, di hydro testosterone (DHT) and DHEA . Typically levels of these hormones are in the NORMAL RANGE, but well above average.
-
•Reduced fertility relating to problems with ovulation in about 40% of women with PCOS.
-
•Increased pigmentation at the back of the neck, inner thighs and abdomen.
-
•Skin tags especially in the axillae and upper inner thighs.
-
•Pre menstrual syndrome ( PMT/PMS) may be more common and more severe
-
•Estrogen dominance i.e. high levels of estrogen compared to progesterone, causing more fat deposition round thighs and butts, worse PMS and some times premenstrual headaches. After the age of 35 it increases the risk of fibroids and very heavy periods, often causing iron deficiency.
-
•Poor self esteem, depression, anxiety and social anxiety are very common in women with PCOS. Women & girls have to battle symptoms like these often without proper support, advice or often the benefit of accurate diagnosis by the medical profession.
For such a common and serious problem PCOS is often not diagnosed or treated properly, and has a major impact on the lives of the women it affects.
Testing for PCOS Spectrum.
If you have several of the symptoms in the list above, you may have PCOS, you should see your doctor and ask for the following tests:
-
•LH/FSH ratio.
-
◦ Luteinising Hormone (LH) & Follicle stimulating hormone (FSH). These are the hormones secreted by your pituitary gland which control the menstrual cycle. If you have PCOS your pituitary gland secretes higher levels of LH throughout the month instead of just before ovulation and ovulation may fail. Therefore LH/FSH ratios are increased to > 1 in women with PCOS.
-
If LH is greater than FSH at any time in the cycle other than ovulation, and there are symptoms of PCOS this woman is highly likely to fit in the PCOS spectrum and benefit from the lifestyle changes. Avoid taking blood tests mid cycle, day 21 is ideal.
LH/FSH ratio may be used to monitor treatment of PCOS. With diet and exercise LH/FSH ratios often fall, and may revert to normal, which seems to equate to higher levels of ovulation, higher levels of fertility and lower levels of male hormones and insulin.
• AMH - Anti Mullerian Hormone is often raised in PCOS Spectrum because of greater number of antral follicles. This hormone falls as women get oldser as their eggs are depleted. It is sometimes known as the “egg timer hormone”.
-
•Testosterone, free testosterone levels, DHT & DHEA. These male hormones are often above average in PCOS, but may fall within the normal range and not be asterisked by the pathology company. Raised DHT may be related to the loss of scalp hair. Excess DHEA from the adrenal gland levels may relate to more severe acne.
-
•Sex hormone binding globulin (SHBG), this protein which usually soaks up male hormone may be decreased in PCOS, especially if there is insulin resistance..
-
• Fasted Serum Insulin levels and fasted blood sugar. Insulin may be increased with PCOS. High insulin levels cause obesity and further increase male hormone levels,
-
•Pelvic ultrasound to look for ovarian cysts. Not all women with PCOS have ovarian cysts.
-
•Estrogen and progesterone levels. Estrogen /Progesterone (E2/PG) ratio is often high in PCOS, even though both hormone levels may fall within the normal range and not be asterisked by the pathology company.
-
•Ferritin levels - low iron stores are common in all women who have periods. I find that a ferritin level of 80 ug/l or more is needed for maximal energy levels, and for scalp hair recovery and fertility. This is despite ferritin levels of down to 25 ug/l being regarded as normal by pathology companies.
-
•It may also be useful to measure Prolactin, a pituitary hormone related to milk production, as excess prolactin can cause irregular periods. Prolactin excess is FAR less common than PCOS however.
-
•Pelvic ultrasound to check for cysts on the ovaries
Treatment of PCOS Spectrum
a. Lifestyle treatments
-
•Early diagnosis. Ideally PCOS should be diagnosed soon after puberty. This allows for education, understanding and acceptance of the condition by the girl and her parents. Early diagnosis allows lifestyle measures to be put in place early, and may avoid depression and anxiety so common with especially teenage PCOS.
-
•Diet. Low GI (Glycaemic Index) , low saturated fat, high fibre diet with plenty of lean protein and vegetables. Eating little and often rather than one or two large meals day is a good strategy. Avoid too many soy products as this can further decrease SHBG levels. Drink heaps of water; aim for 2.5 - 3 litres per day. This type of diet along with exercise helps minimise weight gain, insulin resistance, improves FSH/LH ratio and helps lower male hormones and estrogen/progesterone ratios.
-
•Exercise. Start regular exercise early after puberty and aim for 40 minutes per day 5-6 times a week. Going to the gym, walking, cycling, jogging, swimming, dancing and team sports are all great forms of exercise. Many women with PCOS are excellent athletes and excel especially in sports of strength and endurance e.g. weightlifting, discus and shot-put. Consult a sports teacher or instructor or exercise physiologist to find which forms of exercise will suit you. Regular exercise needs to be an integral long term part of lifestyle for those with PCOS.
-
•Psychological treatment - talking about symptoms, working towards self management, and a good knowledge of lifestyle, herbal and medical treatments allows girls and women with PCOS the full "toolbox" of management strategies to be accessed. Similarly parents and patients should look for signs of poor self esteem, depression or social avoidance and treat these early by focussed strategies or Cognitive Behavioural Therapy by an understanding Psychologist, Doctor or Counsellor. This can avoid serious long term depression and anxiety
-
•Fertility planning. Fertility in women with PCOS tends to fall rapidly after the age of 30. Yet in the early 21st century it is normal for Australian women and couples tend to delay having children till after the age of thirty. As far as women with PCOS are concerned, this causes a BOOM for the IVF clinics, and a lot of angst, heartbreak and expense. I suggest where possible women with PCOS plan to complete having children by their early thirties
Treatment of PCOS should be commenced as early as possible. Diet with low fat and low glycaemic index, combined with a good exercise program, is an essential part of the treatment. See more on diet in our Obesity section. Early diagnosis and close monitoring can help avoid and minimise negative psychological impact of PCOS. Avoid planning on having children too late in life.
b. Herbal/ Vitamin and Mineral Treatments, Cosmetic treatments.
-
• Acne may respond to many over the counter preparations and beauty treatments, these can become very expensive.
-
•Insulin resistance may be helped by chromium 200-1000mg/day, cinnamon and a high fibre diet.
-
•Di hydro testosterone (DHT) levels causing scalp hair loss may be slowed using saw palmetto which inhibits conversion of testosterone to DHT. Avoid saw palmetto preparations with nettle root which may Increase already high free testosterone levels.
-
•Chaste berry (vitex castus agnus) may help PMT by acting in a similar way to progesterone. Evening primrose oil and Vitamin B6 may also help PMT/PMS.
-
•Iron supplements often improve energy levels, fertility and scalp hair - my goal is for a ferritin level of 80ug/l or more. Zinc supplements may also help scalp hair.
-
•Fish oil (EPA/DHA) may benefit cholesterol profile and mood
-
•St Johns Wort, Same and 5-hydroxy-tryptophan may benefit mood
-
•Passiflora Incarnata may benefit anxiety, as may other calming herbs
-
•Excess body hair can be treated by laser, electrolysis or other means.
Integrative Medicine Doctors (AIMA doctors) & Naturopaths often know more about these treatments than many doctors who tend to poo-poo them and move straight to prescription drug treatments, which are effective but may be more prone to long term side effects.
Many doctors still seem to place little emphasis on lifestyle modification, and psychological treatments both of which are the foundation for successful management of PCOS.
c. Drug Treatment for PCOS Spectrum
-
•Oral contraceptive pills, especially Diane, Valette, Yasmin and Yaz. The pill regulates periods and increases SHBG which helps soak up excess male hormone. Diane & Valette may be especially good at helping acne in many women. In my opinion use of the pill should be limited to 2 years for those with PCOS, followed by a break of 6-12 months to see whether periods return when off the pill.
-
•Acne - can be treated with the OCPill as above, and other prescription acne treatments.
-
•Spironolactone is an old fashioned diuretic which helps hirsutism because it has an anti androgen effect. It may take up to 6 months for effects to be noticeable.
-
•Androcur which is a potent inhibitor of 5 alpha reductase, which converts testosterone to more potent DHT in the skin, is occasionally used to limit scalp hair loss in PCOS. It may cause weight gain!
-
•Metformin which was previously not used unless diabetes was present, should be considered earlier when insulin resistance is evident. It may help reduce insulin resistance and help delay the onset of diabetes. In my experience Slow Release Metformin has less side effects especially nausea than other older forms.
-
•Anti depressants especially those not associated with weight gain e.g. Lovan , Zoloft or Cymbalta may greatly improve mood and decrease anxiety.
-
•Bio-identical progesterone in my experience may decrease PMT/PMS, anxiety and mood changes and reduce acne and menstrual headaches, especially if used on days 18 to 28 in women with low progesterone levels i.e. low progesterone/estrogen late in their cycle. Please note that most Australian doctors are not of this opinion, and do not support this however.
More info on PCOS see: http://www.pcosupport.org/
Best Book is "The Low GI Guide to Managing PCOS" by Professor Jennie Brand Miller
Dr David Richardson 2003, revised May 2007 & Feb 2012