
Andropause
male menopause

Dr David Richardson
Andropause (Male Menopause)
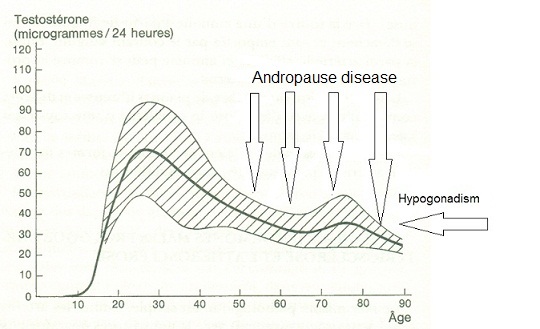
Males undergo menopause too. Hormones in both sexes decline from the early 20's on. Men have no specific marker, such as stopping periods in women, to delineate their menopause. But their hormones decline from the early to mid twenties.
At some point, usually in the early - mid forties this hormonal decline becomes apparent with physical and mental changes occurring.
See “ Male Hormone Checklist” to see how You rate
Some of these changes are:
-
•Increase in abdominal fat
-
•Declining muscle mass and strength
-
•Decrease in motivation and drive
-
•Increase fatigue
-
•Moodiness & irritability ( "Grumpy old man syndrome")
-
•Problems with concentration
-
•Declining interest in sex
-
•Declining spontaneous nocturnal erections
-
•Declining incidence of sexual intercourse
-
•Need for extra stimulation to get erections
-
•Declining ability to sustain erections and declining quality of erections
-
•Increasing tendency for depression
-
•Increase in heart disease
-
•Increase in LDL ("bad") cholesterol
-
•Increasing prostate problems especially BPH
These changes have an enormous impact on men's lives. Their relationships change. Executives lose their aggressive competitive edge and are replaced by younger men. Their interests decline or change. In short they grow old!
Many doctors and endocrinologists deny the existence of andropause, or they measure a man's hormone levels and because they are in the "normal range" , they say that this cannot be the problem. Yet men treated for andropause usually report a decrease in almost all the above symptoms.
What we need to aim for in the treatment of Andropause is a restoration of free testosterone to the normal range for YOUNG MEN, or to keep your free testosterone in the upper third of the range for your age group. From Life Extension Foundation (LEF) data these levels are:
Reference Intervals for Free Testosterone by age from LabCorp (converted to Australian units)
20-29 years
32-92 pmol/l
30-39 years
30-87 pmol/l
40-49 years
25-83 pmol/l
50-59 years
23-75 pmol/l
60+ years
23- 63pmol/l
Why do free testosterone levels decline as men get older??
-
•A protein called SHBG (Sex hormone binding globulin) rises as we age and more testosterone is bound up to it, reducing the amount of available (free) testosterone.
-
•More testosterone is converted to oestrodiol by an enzyme called aromatase.
-
•More testosterone is converted to DHT by an enzyme called 5 alpha reductase.
-
•Less testosterone is made by the ageing testicles.
Prostate Cancer and Testosterone
The biggest fear of doctors, is the fear of Prostate Cancer. Yet there is little evidence that increasing free testosterone levels causes prostate cancer. It is true that testosterone may stimulate an existing prostate cancer which is why all men considering this therapy need a digital rectal examination and measurement of PSA & if PSA is raised, they need a PSA Ratio before embarking on testosterone replacement.
Testosterone replacement may also unmask an early prostate cancer and this will be reflected by a rapid PSA rise in the early stages of treatment . Thus it is wise to perform serial PSA studies six monthly thereafter.
Prostate cancer risk can be reduced greatly by taking nutritional supplements and this is advisable with any testosterone supplementation.
Testing for Andropause
If you have several of the symptoms above, or you score highly in the Andropause Quiz, you may have Andropause; to confirm this we need to rule out other causes of similar symptoms and then test your hormonal status. A full test consists of: (from LEF)
Complete blood count and chemistry profile to include liver-kidney function, glucose, minerals, lipids, and thyroid (TSH)
Free and Total Testosterone
Estradiol (estrogen)
DHT (dihydrotestosterone)
DHEA
PSA
Luteinizing hormone (LH)
Sex Hormone Binding Globulin (SHBG)
It is sensible to test full cholesterol levels as well to help ascertain risk of cardiac disease.
Treatment of Andropause
Not all men need testosterone replacement to treat Andropause, and testosterone replacement will not automatically help all men with Andropause!
The above tests allow us to determine whether your androgen decline is mainly caused by decreasing production of testosterone , or whether the problem is too much SHBG resulting in decreased free testosterone, or too much testosterone conversion to estrogen (via the enzyme aromatase) or too much conversion to DHT (via the enzyme 5 alpha reductase).
Treatment of Andropause may consist of:
-
•Lifestyle and Dietary changes
-
•Nutritional Supplements
-
•Commercial drug therapy
-
•Hormonal supplement with DHEA & sometimes testosterone.
Lifestyle and Dietary changes
-
•Drink more water.
-
•Lose weight - this decreases SHBG & losing abdominal fat reduces estrodiol levels..
-
•Reduce excessive alcohol consumption - this also decreases SHBG.
-
•Regular exercise. In one study men who walked daily were far less likely to develop prostate cancer.
-
•Eat more cooked tomato which contains lycopene which markedly reduces prostate cancer risk.
-
•Eat Cruciferous vegetables such as broccoli, cauliflower, cabbage, and brussel sprouts. These contain Indole 3 Carbinol which increases the conversion of estradiol to “weaker” (2OHE) estrogen. Broccoli also contains quercetin which is beneficial for chronic prostatitis.
Nutritional Supplements
-
•Serenoa repens (Saw palmetto) .Take the herb saw palmetto combined with
-
•Nettle root (Urtica dioica). Saw palmetto and nettle root blocks 5 alpha reductase, reducing the conversion of testosterone to DHT. Nettle root appear to contains substances which bind to SHBG helping reduce the proportion of bound:free testosterone.
-
•Flavenoids. Examples are soy products and red clover. Soy also specifically seems to reduce SHBG by up to 10%, again potentially increasing free testosterone.
-
•Lycopene - greatly reduces prostate cancer risk
-
•Zinc 30mg -50mg/day. Zinc acts as an aromatase inhibitor, potentially reducing the conversion of androgens (male hormones) to oestrogens.
-
•Chrysin is another aromatase inhibitor but is very poorly absorbed from the gut and then may be broken down by the liver. To be effective chrysin needs to be in a cream absorbed though the skin or a troche (lozenge) absorbed though the mucosa of the mouth.
-
•Indole 3 Carbinol which increases the conversion of estradiol to “weaker” (2OHE) estrogen.
-
•Natural progesterone can be used to help block both reductase and aromatase.
-
•Pygeum reduces the binding of DHT to the prostate cells.
Commercial Drug Therapies
-
•Arimidex is a drug which is a potent aromatase inhibitor, but is very expensive. It is used for breast cancer in a dose of 1mg/ day but 1/2mg twice a week may be enough to decrease estrodiol in men according to LEF, meaning a bottle of 28 tablets would last over 6 months. This is an off license use of this drug in Australia and USA. It should only be considered in the presence of high estrodiol levels combined low free testosterone.
-
•Some drug therapies which affect the liver may increase SHBG and therefore decrease free testosterone. Do not stop taking any drug therapy without consulting your doctor.
Hormonal supplement with DHEA & sometimes testosterone.
-
•DHEA is a chemical precursor to testosterone and supplementing this may lead to increased levels of testosterone. The dose of DHEA in men is 50-100mg. In Australia it is available as prescription only and is available only from compounding pharmacists. DHEA should always be taken with zinc to prevent aromatisation to estrone. DHEA supplentation is contraindicated in the presence of prostate cancer.
-
•Testosterone replacement therapy can be given as:
-
1.Sustanon (synthetic testosterone injections) these are effective and are given every two weeks. Disadvantage is that they are metabolised by the liver which may increase SHBG.
-
2.Androderm patches. This is bioidentical testosterone. Two patches need to be worn daily. Major disadvantage is that the patches tend to cause skin irritation, though this can be minimised by using a tiny amount of 1% hydrocortisone cream on the skin before applying the patch.
-
3.Testosterone Implants. These bioidentical testosterone. Major disadvantage is that up to 6 pellets may have to be inserted every 6 months, and that in some men the pellets have a nasty habit of being expelled through the skin a couple of weeks after implantation.
-
4.Natural testosterone given either by cream or troche. These are made by compounding pharmacists. Troches can be made up to contain DHEA and Chrysin & Natural Progesterone as well. They are usually well tolerated and effective. Disadvantage is the expense.
-
5.Oral testosterone tablets or capsules tend to be inactivated by the liver and are poorly effective whilst increasing SHBG.
-
6.Testosterone therapy should be taken along with at least some of the above nutritional supplements to preserve the testosterone and greatly reduce the risk of prostate cancer
When testosterone replacement fails to adequately lift free testosterone levels, re measure SHBG, and salivary testosterone and oestrone (E1) levels to check aromatisation. DHT is hard to assay in Australia.
-
•SHBG may be too high. Ideal SHBG is 13-55 nmol/l.
-
◦SHBG is increased by obesity, excess alcohol, hormones metabolised by the liver (specifically oral contraceptive pills in women) and thyroid disease. It is also increased by the drug Metformin used for diabetics, though this remains the best treatment for obese type two diabetics who need medication. So losing weight and decreasing drinking alcohol are good tactics
-
◦SHBG is reduced by Soy products and higher circulating insulin levels.
-
•Estrodiol is too high. Ideally estradiol should be in the range of 35-105pmol/l for a man of any age. Too much testosterone is being converted to estrone by aromatase. Take zinc and nettle root extract and Chrysin & progesterone ( possibly Arimidex). Take Indole 3 Carbinol to break estrodiol to weaker 2OHE estrogen.
-
•DHT is too high. Ideal DHT level is 0.7- 1.7nmol/l. Take saw palmetto and nettle root plus progesterone to inhibit 5 alpha reductase.
-
•If all of the above are in the ideal range and free testosterone remains low you may not be absorbing testosterone and changing the delivery mechanism e.g. from a troche to a cream may be helpful.